Lac Phan
New member
- Messages
- 12
- Reaction score
- 10
ARTERIOVENOUS MALFORMATION
1.
Definition
There were case descriptions in the nineteenth century by Virchow and
Steinheil in 1895. Cushing and Bailey described the pathology of a small series in
1928 and it was reported the first demonstration of AVM by angi-ography in
1936.
AVMs are inborn deformity injury, including adnomal brain vessels with direct
anastomosis of arteries and veins.They are assumed to appear during fetal
development between the fourth and eighth weeks of life. However, some evidence
suggests that AVMs may develop later in life, as AVMs are rarely detected in utero
or found in infants. One hypothesis maintains that AVMs first appear in utero but
then continue to grow after birth.
2.
Etiology
The precise etiology of AVMs is unclear. Some theories:
− AVMs represent persistent direct connections between arteries and
veins within the primitive vascular plexus.
− AVMs are dynamic and result from a derangement in vessel
growth, i.e., a “proliferative capil-laropathy”.
− AVMs result from a dysfunction of the remodeling process at the
junction between capillariesand veins.
− AVMs have been considered fistulized cerebral venous angiomas.
3.
Histopathological features
➢ Arteries
− AVM arteries are abnormally dilated, with marked thinning in
some regions and degenera-tion or absence of the media and elastic
lamina. Degenerative changes are present, presum-ably due to wall shear
stress caused by high flow. These include irregular thickening of the
vessel wall in some regions, endothelial proliferation, medial
hypertrophy, and multilami-nated, thickened basal laminae.
➢ Nidus
− Nidal vessels may contain a hypertrophic media, blurring the
distinction between arteries and veins.
− Aneurysms and islands of sclerotic tissue may be present within
the nidus.
➢ Veins
− “Arterialized” veins may exhibit thickening of the vein wall due
to cellular proliferation.
− Although thickened AVM veins may grossly resemble arteries,
they lack an organized elastic lamina and therefore are not truly arterial
structures.
− Functional brain tissue is usually not present within an AVM,
although in diffuse lesions, AVM vessels may be separated by normal
tissue.
4. Classification
AVM is classified as follows:
➢ Spetzler-Martin grading based on size, venous drainage,
functional brain region determined on cerebral angiography, CT scan,
MRI.
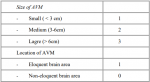
AVM grade = size + eloquence + deep component
➢ Nataf grading
According to the classification of Nataf AVM is divided into 4 grades:
− Grade I: no factor venous proliferation or proliferative circuit.
− Grade II: venous stenosis or venous reflux.
− Grade III: deep venous drainage only.
− Grade IV: aneurysm in or near the nidus.
5. Symptoms
− Hemorrhage
Most common symptom at presentation, occurring in some 53% of patients at
initial diagnosis
− Seizures
After hemorrhage, seizures are the second most common presenting symptom
of intracranial AVMs, occurring in 20–25% of cases.
− Headaches
Headache complaints are more common among patients with AVMs than the
general population suggesting that unruptured AVMs may cause headaches.
− Developmental learning disorders
Patients with AVMs are more likely to have developmental learning disorders
than patients with other intracranial disorder, even many years prior to the
diagnosis of the the AVM
6. Treament
− The principles of treament:
The primary goal of AVM treatment is to completely remove the AVM from
the circulation, preventing future bleeding, while minimizing the risk of
complications and complications from treatment.
− Treament: there are 5 Management options
1. Expectant management
2. Surgery
3. Radiosurgery
4. Embolization
5. A combination of embolization, radiosurgery, and/or surgery
References
- Mark R. Harrigan, Jonh P. Deveikis, “Handbook of Cerebrovascular
Disease and Neurointerventional Technique”, Third Edition.
- James Vincent Byrne, “Tutorials in Endovascular Neurosurgery and
Interventional Neuroradiology”, Second Edition.
- Robert F. Spetzler, M.D., And Neil A. Martin, M.D. Division of
Neurological Surgery, Barrow Neurological Institute, “A proposed
grading system for arteriovenous malformations”.
- Chi Cuong Tran PhD, Luu Giang Nguyen MS, “Chẩn đoán và điều
trị bệnh mạch máu thần kinh và đột quỵ.”
1.
Definition
There were case descriptions in the nineteenth century by Virchow and
Steinheil in 1895. Cushing and Bailey described the pathology of a small series in
1928 and it was reported the first demonstration of AVM by angi-ography in
1936.
AVMs are inborn deformity injury, including adnomal brain vessels with direct
anastomosis of arteries and veins.They are assumed to appear during fetal
development between the fourth and eighth weeks of life. However, some evidence
suggests that AVMs may develop later in life, as AVMs are rarely detected in utero
or found in infants. One hypothesis maintains that AVMs first appear in utero but
then continue to grow after birth.
2.
Etiology
The precise etiology of AVMs is unclear. Some theories:
− AVMs represent persistent direct connections between arteries and
veins within the primitive vascular plexus.
− AVMs are dynamic and result from a derangement in vessel
growth, i.e., a “proliferative capil-laropathy”.
− AVMs result from a dysfunction of the remodeling process at the
junction between capillariesand veins.
− AVMs have been considered fistulized cerebral venous angiomas.
3.
Histopathological features
➢ Arteries
− AVM arteries are abnormally dilated, with marked thinning in
some regions and degenera-tion or absence of the media and elastic
lamina. Degenerative changes are present, presum-ably due to wall shear
stress caused by high flow. These include irregular thickening of the
vessel wall in some regions, endothelial proliferation, medial
hypertrophy, and multilami-nated, thickened basal laminae.
➢ Nidus
− Nidal vessels may contain a hypertrophic media, blurring the
distinction between arteries and veins.
− Aneurysms and islands of sclerotic tissue may be present within
the nidus.
➢ Veins
− “Arterialized” veins may exhibit thickening of the vein wall due
to cellular proliferation.
− Although thickened AVM veins may grossly resemble arteries,
they lack an organized elastic lamina and therefore are not truly arterial
structures.
− Functional brain tissue is usually not present within an AVM,
although in diffuse lesions, AVM vessels may be separated by normal
tissue.
4. Classification
AVM is classified as follows:
➢ Spetzler-Martin grading based on size, venous drainage,
functional brain region determined on cerebral angiography, CT scan,
MRI.
AVM grade = size + eloquence + deep component
➢ Nataf grading
According to the classification of Nataf AVM is divided into 4 grades:
− Grade I: no factor venous proliferation or proliferative circuit.
− Grade II: venous stenosis or venous reflux.
− Grade III: deep venous drainage only.
− Grade IV: aneurysm in or near the nidus.
5. Symptoms
− Hemorrhage
Most common symptom at presentation, occurring in some 53% of patients at
initial diagnosis
− Seizures
After hemorrhage, seizures are the second most common presenting symptom
of intracranial AVMs, occurring in 20–25% of cases.
− Headaches
Headache complaints are more common among patients with AVMs than the
general population suggesting that unruptured AVMs may cause headaches.
− Developmental learning disorders
Patients with AVMs are more likely to have developmental learning disorders
than patients with other intracranial disorder, even many years prior to the
diagnosis of the the AVM
6. Treament
− The principles of treament:
The primary goal of AVM treatment is to completely remove the AVM from
the circulation, preventing future bleeding, while minimizing the risk of
complications and complications from treatment.
− Treament: there are 5 Management options
1. Expectant management
2. Surgery
3. Radiosurgery
4. Embolization
5. A combination of embolization, radiosurgery, and/or surgery
References
- Mark R. Harrigan, Jonh P. Deveikis, “Handbook of Cerebrovascular
Disease and Neurointerventional Technique”, Third Edition.
- James Vincent Byrne, “Tutorials in Endovascular Neurosurgery and
Interventional Neuroradiology”, Second Edition.
- Robert F. Spetzler, M.D., And Neil A. Martin, M.D. Division of
Neurological Surgery, Barrow Neurological Institute, “A proposed
grading system for arteriovenous malformations”.
- Chi Cuong Tran PhD, Luu Giang Nguyen MS, “Chẩn đoán và điều
trị bệnh mạch máu thần kinh và đột quỵ.”